Your pharmacy foundation year is the final stage of training before you’re a qualified pharmacist. But what exactly can you expect during your time as a foundation pharmacist? What will your key responsibilities be, and how will they prepare you for life as a fully fledged pharmacist?
In this article, Adam Gardener and Fariea Hussain share their experiences as foundation year pharmacists with Gateshead Health NHS Trust, where rotational pharmacists are each allocated two wards to work on. That might sound like a lot of responsibility while you’re still training, but knowing what to expect and some top tips for managing your workload can make the job a lot easier.
Adam and Fariea each shared their five tips they wished they’d known before starting their foundation year:
Adam’s top tips
Fariea’s top tips
Firstly, let’s recap how to become a hospital pharmacist in the UK. To become a fully qualified hospital pharmacist, you need to:
Hospital pharmacists are ultimately responsible for dispensing medications used within the hospital environment. This encompasses a wide range of tasks, including:
From learning to prioritise the most critical tasks to communicating clearly and knowing how to navigate ‘blind areas’, Adam and Fariea explain what your role and responsibilities will look like as a foundation hospital pharmacist.
At the start of each shift, make sure you’re well organised and know your commitments for the day. Do you have dispensary or operational commitments (such as controlled drug (CD) checks or mandatory training), or do you have teaching or other responsibilities?
Communicate with the staff you’re working with every day to identify who may need support and who is available. Building a good relationship with the other pharmacy staff will enable you to complete tasks more effectively and efficiently during your time on the ward.
Depending on your Trust, there may be a prioritisation system in place to identify patients who need medicines reconciliation or pharmacy review. Building prioritisation into your day-to-day workload will help ensure efficient and safe working. Bear in mind that priorities may change depending on the clinical area you are working in. Therefore, it’s a good idea to know which doctors, nurses and allied healthcare professionals are looking after which patients that day, so any questions can be directed straight to them.
Medicines reconciliation
At Gateshead Health NHS Trust, medicines reconciliation for patients on high-risk medications are prioritised first, followed by patients in order of time since admission. It’s crucial to get medicines accurate from the start of someone’s admission to reduce any risk of incorrect medicine administration and further work later in someone’s stay.
High-risk prescriptions
If any new patients are on high-risk medications, try to see these patients near the beginning of the day, so you can ensure their medications are prescribed correctly, and you have time to make amendments with the prescriber if required. This also gives you time to order the medications if they haven’t brought their own in from home.
Ward priorities
Looking at when a patient was last reviewed will guide you as to when they need to be seen. If the patient has been reviewed within the past one or two days and is stable, then these reviews can wait until the higher risk reviews are completed.
Gateshead Health NHS Trust uses an internal prioritisation system known as the ‘ward dashboard’. This system flags key criteria unique to the pharmacy team, including:
The system also retains information between hospital admissions, such as if a patient is on any high-risk medications, and if the patient has a dosette box, including which pharmacy supplies this. The dashboard enables workload planning and prioritisation, and establishes a way of seeing all high-risk patients.
Supporting your team
When prioritising the day’s workload, think of your team and colleagues; are there any pharmacy technicians or pharmacy assistants on your team? Depending on your Trust they may have different roles, skills or tasks they can help with. Utilising the skillset of the team and delegating accordingly will reduce your workload and improve patient care.
If you’re struggling with the workload, don’t be afraid to ask for some support on the ward; we’ve all been there when first starting out, but once you get used to the usual workload, you’ll learn how to manage your day.
Perhaps the most varied and unpredictable part of a hospital pharmacist’s day comes from clinical queries. These can come from a range of ward staff, including consultants, junior doctors, nurses and other members of the pharmacy team.
At first, being called or approached with a query can be daunting, but remember, if someone else is asking the question, then they don’t know the answer either! Once you take a moment to process the question and can provide the answer, you get a feeling of pride and gratitude that the hard work you put in while training has paid off.
However, there will inevitably be times that you don’t know how to answer a query. In these situations, you need a clear process in your mind of how to approach the problem. The topic of the question will dictate the order in which a problem can be solved. Sometimes, a simple check of a medications monograph can supply the answer. On other occasions, the questions may be more complex, and you might need to ask a more senior pharmacist. The natural reaction is to provide an answer immediately, but the best way to deal with questions is to take your time.
At Gateshead, the pharmacists have been really helpful and responsive whenever we have called with queries (and there have been a fair few – thanks everyone!). There is nothing wrong with discussing your query with a senior or another colleague before providing your answer. Think through your options and construct a logical plan.
If you receive a call, it’s more than reasonable to take notes, ask for a contact number, and call back later with the information. If you’re approached on the ward, ask if the information is needed urgently for an acute scenario. If it isn’t, establish a period you can work to. It’s important to use this time wisely, considering as many angles as possible to pre-empt any additional or follow-up questions.
The more time you take researching your question, the more you can ensure that your answer is the most appropriate. If you’re able to justify your decision and have documented your reasoning in a clear and concise manner, demonstrating your thought process, then you’ve done your due diligence and can be confident in your answer.
It can be humbling to accept that you don’t know everything, but this grounds you as a pharmacist. Experience will provide you with a great deal of knowledge that can be applied to a range of situations; when beginning a career as a pharmacist, using your seniors for advice is an accessible and reliable point of contact. They have the clinical knowledge coupled with the practical aspects that are unique to each hospital, often offering more practical help than any guideline or monograph.
To maximise opportunities when consulting a senior colleague, take the chance to ask for some clinical supervision. One-to-one time discussing a case can teach you a great deal of practical and clinical details. It is often the case that after qualifying, some problems are over-thought and worried about, while other topics may be more serious or essential than previously thought.
Applying the Johari’s window model to your clinical knowledge helps you to analyse what knowledge is known and unknown to yourself and others, and can be superimposed to look at your own knowledge.
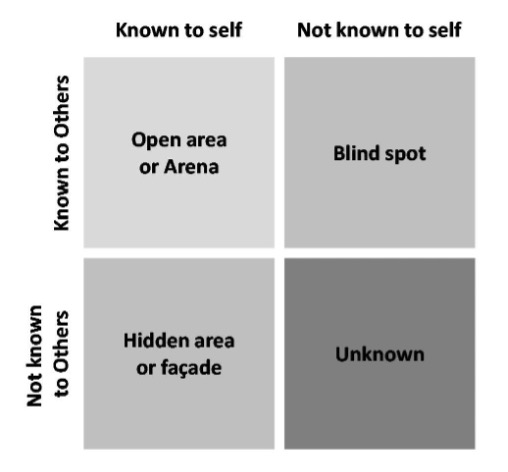
Using this tool can increase your self-awareness of ‘knowing what you know’. Opportunities to learn about topics in the unknown area arise daily and can be used to continue your professional development. We encourage researching new concepts you come across and discussing these with your peers and seniors to consolidate your learning and fill in any gaps.
Navigating a blind area
Adam explained: “While working on a care of the elderly (COTE) rotation, I encountered a patient on raloxifene for the first time. Raloxifene is a medication licensed for the treatment and prevention of osteoporosis in postmenopausal women.
“I conducted my established routine of clinical checks and recommended some changes to optimise the patient’s treatment. Being unaware of the medicine, I asked a more senior colleague on the ward to check my work and offer any further suggestions. Here, I was taught of the high VTE risk associated with the medication. I read the SPC and educated myself further and suggested the suspension of the medication during the period of acute illness.”
Navigating a hidden area
Fariea shared: “I was asked for some help prescribing eltrombobag by one of the ward doctors. I had come across this once during my pre-reg year, but couldn’t remember the specifics of it. I asked a colleague if they would mind reviewing the patient with me and could help me with the query.
“When it was discussed that this medication was for the treatment of thrombocytopenia, I recalled that this medication interacts with many electrolyte replacement medications. The patient was on both magnesium and calcium supplements so, after discussing with my colleague, I suggested what the optimal timings of medications would be to best prevent any occurrence of drug interactions.
“I had forgotten I had dealt with this medication in the past, but after hearing its indication, I remembered some information regarding it.”
Screening discharge prescriptions may make up a significant amount of a foundation year hospital pharmacist’s workload, especially in the afternoon. Ensuring a person’s medication is accurate on leaving hospital is key for safety and continuity of care.
In some clinical areas, there may be a ward round or handover towards the middle of the day; this is where the whole multidisciplinary team (MDT) get together for an update on all patients on the ward. Attending these handovers is not only a good way to hear which patients will be going home, but also emphasises that there is a pharmacy presence on the ward. These can also be a good opportunity to raise outstanding pharmacy jobs or queries.
Some wards may have a discharge coordinator who is responsible for facilitating the appropriate discharge of a patient, particularly for those who need district nurses, packages of care or social referrals. Liaise with them or the nurse in charge if you have any questions regarding who is being discharged. Knowing who is going home in advance of the script being written allows you to clinically screen the medication and counsel patients on new medications. If you’re confident in the plan, you could order any medicines required in advance.
Depending on the number of discharges and clinical queries you get asked throughout the day, you may not always complete all of the ward reviews you wanted to that day. Don’t be disheartened if this is the case. By prioritising your reviews as previously stated, you can rest assured that the high-risk patients have been seen and the patients on your ward are clinically safe at the end of the day.
Pre-emptive discharges
Pre-emptive discharges can sometimes be tricky, as medications can be added at the last minute. Consider cases on an individual basis if it is appropriate to act proactively. We wouldn’t advise pre-empting any discharge that requires a new dosette box for the patient or contains control drugs. Like with medicines reconciliation, use any technicians or assistants you have available to support. This frees up your time, so you can focus on the clinical screening of the discharge prescriptions.
Get support throughout your career when you become a UKCPA member. Join as a trainee pharmacist for free to access extensive resource libraries, discussion forums, expert-led training courses, and networking events. Once you’re a qualified pharmacist or pharmacy technician, membership is less than £3 a week.
The opinions expressed in this article are those of the author. They do not purport to reflect the opinions or views of the UKCPA or its members. We encourage readers to follow links and references to primary research papers and guidance.
This article is based on an original article written by Fariea Hussain and Adam Gardener who worked as rotational pharmacists at Gateshead Health NHS Foundation Trust.
Join UKCPA for less than £3 a week and access all our communities, education and resources.